Back to 2024 Posters
Open Bypass Is Associated With Better Amputation-Free Survival Than Endovascular Therapy in High Surgical Risk Patients With Chronic Limb Threating Ischemia: Inverse Probability of Treatment Weighting Analyses
Mohammed Hamouda
1, Mikayla Kricfalusi
2, Sina Zarrintan
1, Sherene Shalhub
3, Mahmoud Malas
1 1University of California San Diego, La Jolla, CA;
2California University of Science and Medicine, Colton, CA;
3Oregon Health & Science University, Portland, OR
BACKGROUND:Limb salvage in patients with chronic limb threatening ischemia (CLTI) require revascularization whether by open surgical bypass [preferably using single segment great saphenous vein (SSGSV)] or endovascular therapy (ET). ET has been considered to be safer option in patients with high surgical risk compared to open bypass. The aim of this study, is to investigate the one-year outcomes of SSGSV vs ET in each risk cohort in multi-institutional national cohort to investigate which procedure is safer for each high-risk group.
METHODS:The Vascular Quality Initiative (VQI) infrainguinal bypass and peripheral vascular intervention datasets were queried for all patients who underwent lower extremity revascularization for CLTI from 2016 to 2023. Our exposure groups were patients who underwent 1- Open bypass using SSGSV and 2- ET. Patients with prior ipsilateral revascularization (open/ET), major amputation (MA), or concomitant procedures were excluded. We used inverse probability weighted (IPW) Cox regression analysis (based on propensity scores) to compare one-year freedom from major amputation (MA) or death in SSGSV vs ET. The covariates in our models include demographic data, level of revascularization (femoropopliteal, infrapopliteal, femorotibial), medical and surgical comorbidities, indication (rest pain, tissue loss), preoperative and discharge medications, and operative characteristics. Hazard of MA/death in SSGSV vs ET was recorded in each of the following high-risk groups: age>75, insulin-dependent diabetes, dialysis, recent myocardial infarction (MI), positive stress test (PST), BMI>40, chronic obstructive pulmonary disease (COPD), and non-ambulatory status.
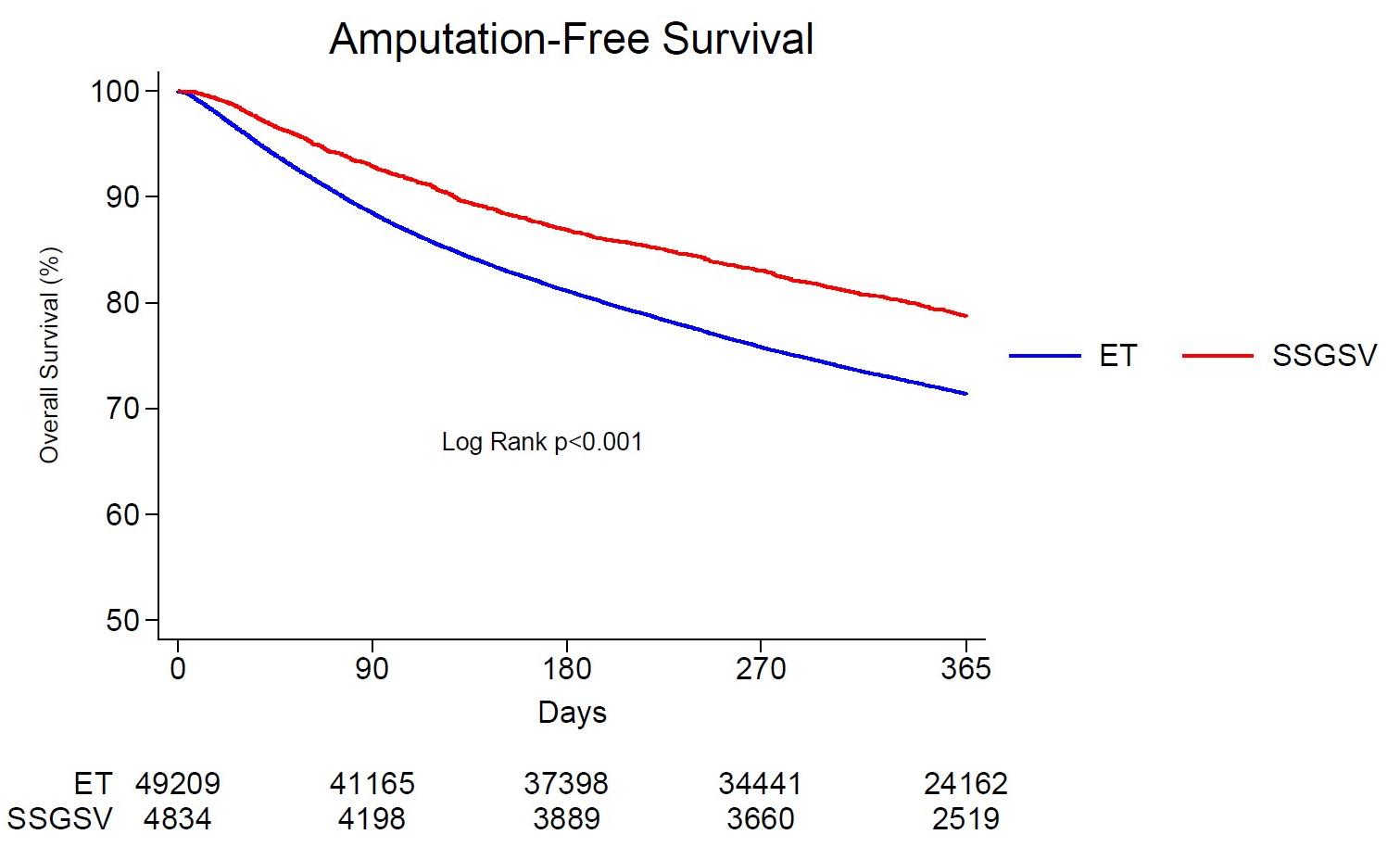
RESULTS:A total of 65,699 patients were included: SSGSV 6,959 (10.6%) and ET 58,740 (89.4%). Compared to ET, SSGSV was associated with decreased hazard of MA/death at one year in patients who are over 75 [aHR=0.77 (95%CI=0.68-0.87), p<0.001], with insulin-dependent diabetes [aHR=0.86 (95%CI=0.78-0.95), p=0.003], on dialysis [aHR=0.79 (95%CI=0.68-0.92), p=0.002], with COPD [aHR=0.76 (95%CI=0.68-0.87), p<0.001], and those who were non-ambulatory [aHR=0.69 (95%CI=0.57-0.83), p<0.001] (Table I). On the other hand, there was no significant difference among both revascularization procedures regarding one-year amputation-free survival in patients who experienced a recent MI (within 6 months), as well morbidly obese patients (BMI>40) and those with a positive stress test prior to intervention (p>0.05). Figure-1 demonstrates greater freedom from MA/death in patients with one or more of the aforementioned risk factors who underwent open bypass compared to ET.
CONCLUSIONS:In this large multi-institutional study, open bypass with SSGSV was clearly associated with superior amputation-free survival at one year compared to ET in patients considered at high surgical risk (over 75, insulin-dependent, on dialysis, with COPD and non-ambulatory. This challenges the common notion of ET being less invasive and safer for these vulnerable patient cohorts. ET can be an acceptable alternative to open bypass in morbidly obese patients and those with a positive stress test or a recent MI.
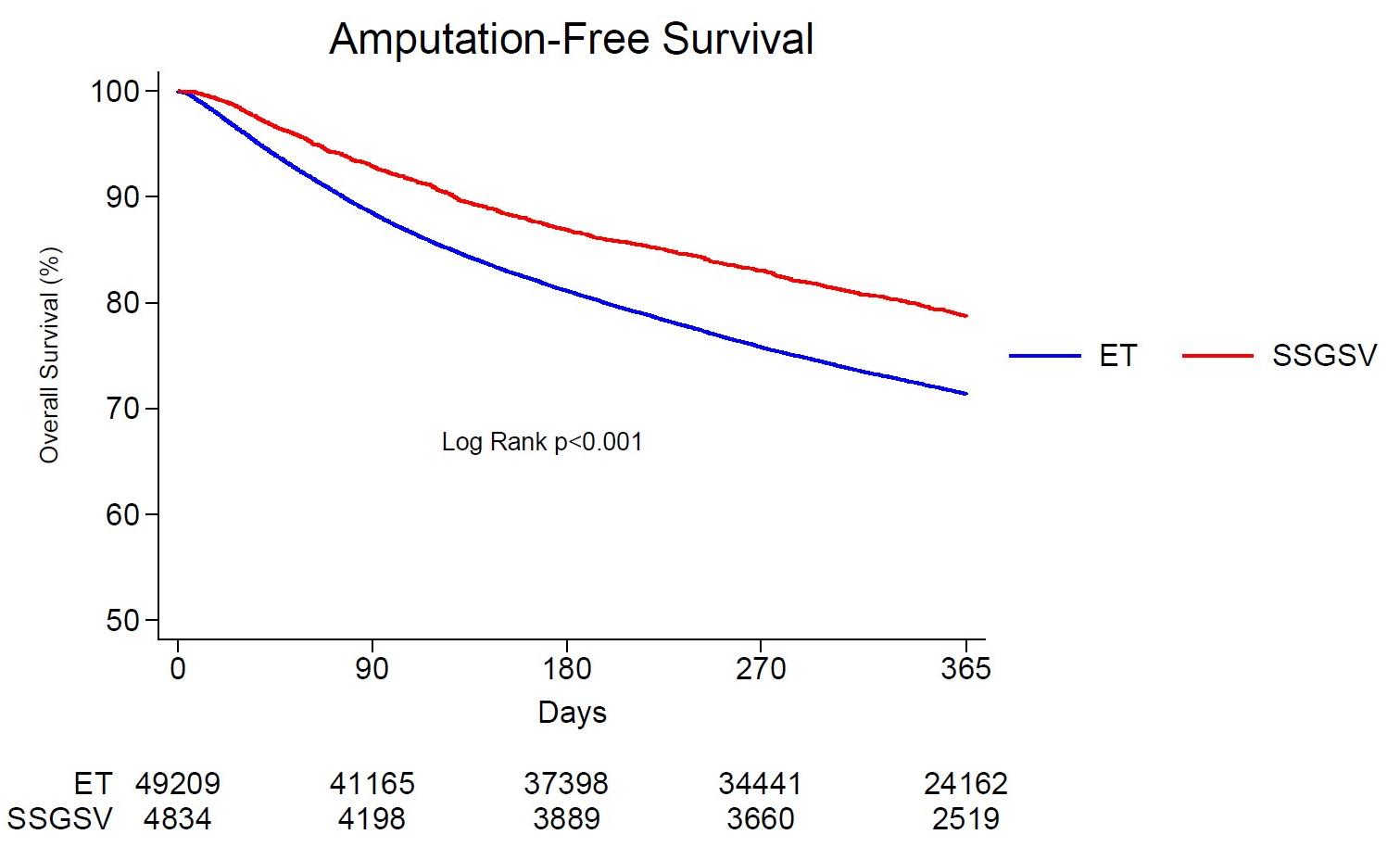
Table I: IPW One-year outcomes of SSGSV bypass versus ET (reference) stratified by risk group | aHR | 95% CI | P-value |
| [reference group = ET] | | |
| Age>75 | 0.77 | 0.68-0.87 | <0.001 |
| Insulin-dependent Diabetes | 0.86 | 0.78-0.95 | 0.003 |
| Dialysis | 0.79 | 0.68-0.92 | 0.002 |
| Recent MI (<6 months) | 0.83 | 0.55-1.24 | 0.355 |
| Positive Stress Test | 0.88 | 0.74-1.04 | 0.123 |
| BMI>40 | 0.84 | 0.59-1.22 | 0.363 |
| COPD | 0.76 | 0.66-0.88 | <0.001 |
| Non-ambulatory | 0.69 | 0.57-0.83 | <0.001 |
Back to 2024 Posters